The French Reprocessing Revolution
Will Europe Pass the US in Healthcare Sustainability and the Use of Reprocessed Devices?
When FDA in 2000, as the first country in the world regulated the use of reprocessed single-use devices, they responded to concerns from manufacturers and physicians that un-regulated re-use of single-use devices could compromise patient safety. Regulation meant that unsafe reprocessing in hospital sterile processing departments stopped – and that third-party reprocessing companies got a regulatory path for reprocessing, so that hospitals could gain financial benefit from device re-use without compromising patient safety. It also - by accident - meant that US healthcare became more prepared to address climate change concerns: While regulated reprocessing saves hospitals hundreds of thousands of dollars every year, it also dramatically reduces the hospital’s CO2 emissions.
Life-Cycle Analyses comparing the carbon footprint of new electrophysiology (EP) devices with the carbon footprint of new EP devices have demonstrated that the carbon footprint of a reprocessed device is half the footprint of a new device (Schulte et al., 2021). Using an EP device instead of a new one reduces the environmental impact by almost 2 lbs CO2 equivalent.
On the other hand, we have seen recycling programs put in place in electrophysiology. However, from an environmental perspective, compared with reprocessing, recycling is a far less valuable solution than reprocessing. EP devices collected to be recycled will not be re-used, but rather broken apart, and the recyclable parts (about 30% of residual hospital waste) will be used in the manufacture of other products. If, instead, the catheters were being reprocessed, the entire catheter is salvaged and made available for another use with the use of very few resources. Since most single-use EP catheters can be reprocessed and re-used, putting in place a recycling program simply means that the environmental benefit is lessened. The average EP lab can reduce their CO2 emission by more than 2,200 pounds CO2 equivalent per year through reprocessing. This impact is significantly reduced with a recycling program which implies that a new catheter will be needed. In other words: Every time a catheter is recycled rather than reprocessed, the EP lab increases CO2 emissions.
Every time a catheter is recycled rather than reprocessed, the EP lab increases CO2 emissions.
In short, reprocessing has emerged as a prime solution for addressing the need for healthcare to reduce its carbon footprint, and the US FDA became an (unknowing) early champion for reducing healthcare’s carbon emissions footprint. The US has, if you will, been ahead of the rest of the world. This may be changing, and there is great risk that the US will be left behind other countries, particularly in Europe, in its efforts to make healthcare more “climate friendly”.
In the UK, for example, the National Health Services (NHS) has aggressively engaged in healthcare sustainability efforts with mandates to implement and prefer more sustainable solutions – including single-use device reprocessing. In France, the Working Group of Cardiac Pacing and Electrophysiology of the French Society of Cardiology recently published a position paper on sustainability in electrophysiology that presents a solution that represents a more deliberate and far-reaching model than anything we have seen in the US (Sacher et al, 2024).
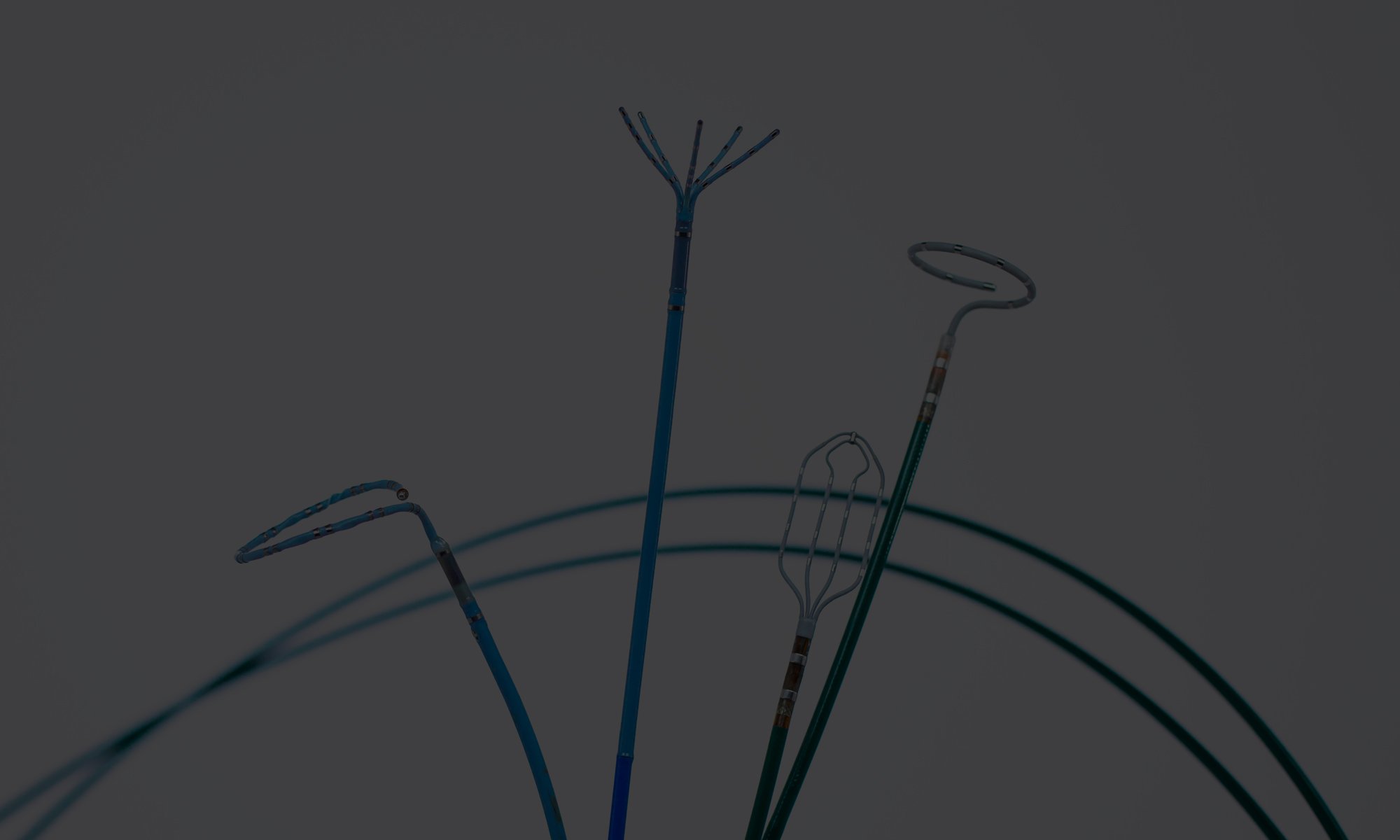
The position paper points at why looking at sustainability in EP is particularly important: EP mainly uses high-tech, single-use medical devices, as opposed to other procedure areas, where reusable, low-complexity devices dominate. In EP, rare metals and rare-earth elements are crucial for manufacturing devices, and the materials are sourced from a complex network of suppliers and locations around the world. The fragile nature of this materials supply network has already had an impact on EP procedures in France as well as in the US, such as when chip shortages lead to cancelled procedures. Moreover, Atrial fibrillation procedures have a carbon footprint of 170 lbs of carbon, with material production and manufacturing contributing 71% of this. This means that reprocessing, which re-uses these parts, has a significant impact on the carbon footprint. Additionally, EP procedures grow by 10-15% every year in the US as well as in Europe, and due to the use of scarce materials, the supply of these devices may eventually itself become a problem – a problem that could partially be addressed through reprocessing.
The authors of the positioning paper declare that “Reprocessing of certain single-use medical devices appears to be a solution for reducing supply tensions, limiting the environmental impact of medical devices (carbon footprint and reduction of raw material extraction) and lowering procedural cost”. This is a compelling statement by a society of cardiologists. Reprocessing is still prohibited in France, but it is noteworthy that the clinical community, which has traditionally been the most hesitant to adopt reprocessing, is now pushing for the practice to be established – they are more progressive than the French authorities.
The key risks associated with reprocessing – loss of functionality and contamination – are also addressed, but the authors reference studies to conclude that “[…] neither the material properties nor the functional characteristics of the devices were altered as a result of reprocessing. Moreover, the reprocessed catheters did not disadvantage patients or medical doctors […] and , reuse of electrophysiology catheters was considered safe for patients”. Interestingly, the authors warn that “[…] some electrophysiological devices are equipped with lumens (sheaths, irrigated catheters, needles), and precautions should be taken because some areas can be difficult to reach. Cleaning and sterilizing the lumens as well as checking that there is no obstruction or leak are essential. Thus, medical devices with lumens should probably only be reprocessed by facilities with dedicated expertise”. Innovative Health holds several patents on micro-lumen cleaning and inspection as well as several FDA clearances for devices with micro-lumens. Since more and more devices are designed with lumens, the evolution of reprocessing technology that can clean and inspect these is becoming more and more important every day.
Innovative Health holds several patents on micro-lumen cleaning and inspection as well as several FDA clearances for devices with micro-lumens.
In the US, substantial numbers of diagnostic catheters, sheaths, cables, etc. are being reprocessed and re-used. The use of reprocessed mapping catheters is more rare (due to manufacturer interference) and no ablation catheters have been cleared for reprocessing. Both from an environmental and from a fiscal perspective, this means that the potential for reprocessing is far from realized. In fact, in an Atrial Fibrillation procedure, those two catheters typically represent more than 50% of the device costs. In contrast, among French physicians, “The reuse of mapping and ablation catheters emerged as the solution mentioned most frequently by physicians”.
The position paper is not only far-reaching in its recommendations for reprocessing EP devices, it is also realistic about barriers to increasing sustainability in EP. The authors present a framework for how the multiple stakeholders involved (country, manufacturer, medical society, hospital and physician) need to action to create meaningful change. National authorities must mandate LCA analyses for devices and establish carbon emission programs such as the NHS program. Manufacturers should start reprocessing their own devices(!). The medical societies should integrate carbon emission footprint in scientific meetings, and the hospital should integrate carbon emissions into the process of selecting which devices to use.
FDA’s regulation of single-use device reprocessing effectively made the US the leader in EP sustainability efforts early on. However, in spite of the role the environment plays healthcare and in the US society in general, very little has been done to build on this early leadership. As a result, we will likely have to look abroad to witness improvements in the sustainability of EP procedures. And the charge is led by an unlikely group: Should the collective opinion of French electrophysiologists shape future re-use practices in France, they will be decades ahead of the US in terms of EP sustainability and financial responsibility!
References:
A. Schulte, D. Maga, N. Thonemann (2021). Combining life cycle assessment and circularity assessment to analyze environmental impacts of the medical remanufacturing of electrophysiology catheters. Sustainability 13(2).
Frederic Sacher et al. (2024). Position paper on sustainability in cardiac pacing and electrophysiology from the Working Group of Cardiac Pacing and Electrophysiology of the French Society of Cardiology. Archives of Cardiovascular Diseases, the French Society of Cardiology. January 2024.