Not All Reprocessors Are Created Equal
Industry Fragmentation
The October 2023 FDA “warning letter” CMS# 664014 to Renovo, Inc. DBA Provision Device Reprocessing Solutions in Bend, Oregon concerned itself with quality violations associated with the company’s sale of new models of previously cleared 510(k)s, which FDA said required new 510(k)s. The working letter is based on a form FDA 483 “List of Inspectional Observations”, noting non-compliance with Quality System regulations and marketing new, unapproved devices. The medical devices were “adulterated” (lacked approval of a premarket approval application) and “misbranded” (lacked a cleared 510(k)).
What does this mean? When a reprocessing company, such as Renovo, wants to reprocess a single-use marked medical device, they have to go to FDA and demonstrate that they can clean, inspect and test the device to a point where FDA can determine the device does not come with added patient risk or concerns about functionality, as compared with a new device. Then FDA issues a 510(k) – a clearance to reprocess and sell the device to healthcare facilities.
If different versions of the device exist or are launched after this clearance has been granted, the company can examine these devices to ensure they can be cleaned, inspected and tested just as well as the device included in the clearance – and then make a “note to file” that these new or different versions will be subsumed under the original FDA clearance.
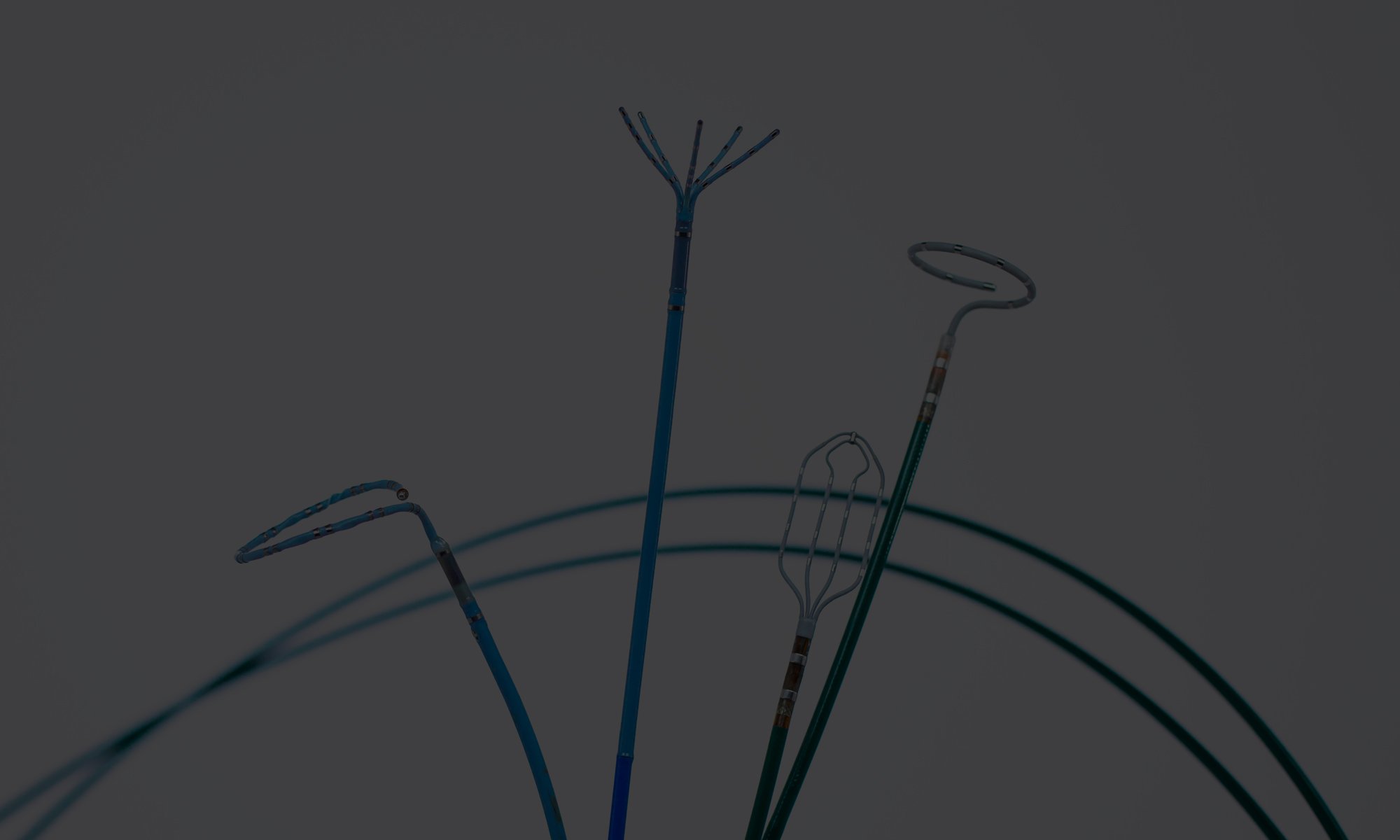
It makes a lot of sense. Medical device companies constantly issue new versions of their devices. You get a reprocessing clearance to reprocess a device with a blue shaft. Next year a new version is launched with a red shaft. If that is the only difference, you can safely reprocess the red-shafted device without adding patient risk or compromising functionality of the device.
However, responsible reprocessing companies are on high alert when this examination takes place. Does the different version have a different indication for use? Is the instrument longer than the cleared device? Does it have different imaging components? Is the lumen smaller? All of these can mean that the cleaning, inspection, and testing put in place for the original device just are not good enough to ensure the new/different device is safe.
In FDA’s warning letter, the agency explains: “These new models are […] versions of OEM (original equipment manufacturer) models that were not included in [the cleared 510(k)]. The additional OEM models have smaller diameter shafts, smaller diameters lumens, smaller tip elements, and/or longer shafts than the OEM models included in [the 510(k) number], and they present a more challenging scenario for cleaning and re-sterilization compared to the designs of the OEM models that were included in [the 510(k) number]. Your company did not evaluate how cleaning and re-sterilization of the additional OEM models with different designs could affect the performance specifications and reliability of your new . . . models. These changes could significantly affect the safety or effectiveness of the . . . devices and required the submission of a new 510(k).”
Think about it. I can demonstrate that I can safely clean and inspect a 0.05 cm diameter lumen. A new model is launched with a 0.02 cm diameter lumen. I can’t simply assume that I can clean and test this the same way, since the new lumen is much smaller. I may not even be able to inspect the device visually. So, I cannot be sure there is not fragments of plastics or organic matter inside the lumen. Even to a layman, this is wrong. It clearly implies risk for patient safety.
It clearly implies risk for patient safety.
When reprocessing companies make use of “notes to file” to “extend” a clearance to cover models or versions of a cleared device not originally included, it is because they can ascertain that requirements to clean, inspect and test the new/different version are the same or less than for the cleared device. That’s the case (for example) of a 0.08 cm version being launched. Since the lumen is larger than the lumen of the cleared device, I can be sure that I can safely clean, inspect, and test the device. The same logic applies to devices with different shaft lengths, for example.
Responsible reprocessors will typically seek clearance for the “worst case scenario” model of a device. If the device comes with 0.02 cm, 0.05 cm, and 0.08 cm lumens, the responsible reprocessor will seek clearance to reprocess the 0.02 cm lumen, then do “notes to file” (after careful examination) to “extend” the clearance to cover the 0.05 cm and 0.08 cm device. This does not work the other way around.
I have previously written about the danger associated with new reprocessing companies coming to market without the legal, ethical, and operational stance that has formed the reprocessing industry: “In an FDA submission, transparency and data integrity is important. The reprocessor should only apply for the products and brands that data supports. The rule is that you cannot include two devices in a submission that have different indications or material design/functionality differences. There have, recently, been situations where clearances have come very easily to new reprocessors, and it could be speculated that “creative” work is the cause. And when the reprocessor utilizes its clearance, you should expect them to be conservative about what devices they consider to fall under that clearance.”
Renovo’s conduct here is wrong, and I want everybody to think about exactly how wrong it is. Their decision could theoretically lead to patient harm because of dangerous device malfunction. FDA did right in issuing the warning letter, and as a member of the industry, I am thankful for the role FDA plays here.
Renovo’s conduct here is wrong, and I want everybody to think about exactly how wrong it is.
In single-use device reprocessing, there are two types of players: 1) Companies organized under the Association of Medical Device Reprocessors (AMDR); and 2) Those that are not.
As a member of AMDR, a reprocessing company follows the guiding principles of safe reprocessing and must adhere to rules about quality, compliance, and ethics in marketing. And AMDR members must be single-mindedly concerned with helping hospitals reduce costs and environmental impact, without consideration for profits on other product lines.
In reality, AMDR members go further than that and constantly work to improve healthcare’s understanding of the value of medical device reuse. As an example, last year, AMDR member Stryker Sustainability Solutions published Life Cycle Assessment (LCA) studies for 5 different devices that demonstrated how the carbon emissions footprint of a reprocessed device is significantly lower than the carbon emissions footprint of a new device. Similarly, Cardinal’s Sustainable Technologies (also an AMDR member) funded a study to demonstrate the difference in carbon emissions footprint between a reprocessed and a new IPC sleeve – with similar findings.
This type of activity shines a light on differences that make a difference in an industry that is increasingly fragmented. I implore you – not as a “salesperson”, but as somebody who takes pride in an industry that has always put patient safety first – to think about what reprocessor to work with. Look for the AMDR logo.