Moving Cardiology Procedures into the Surgery Center: A Long Journey Ahead
Ambulatory Surgery Centers (ASC) are facilities that offer patients a convenient location out of the hospital to have surgical procedures performed. The adoption of surgical centers was centered around a model that provides convenient high-quality services to patients while simultaneously demonstrated a reduction of cost. The success and growth of Ambulatory Surgery Centers over the last ten years has demonstrated that the move to outpatient procedure settings is here to stay. Most healthcare organizations have begun to double down on their commitment to expand services in the outpatient setting with a focus on ASC service lines. Expansion by CMS of approved procedures over the last 5 years has assisted with this move to the outpatient setting. This year, CMS slowed this expansion with an obvious step backwards: Plans to cut procedures from the ASC list and take a deeper look at what procedures should not be moved into the ambulatory setting and remain in the inpatient setting.
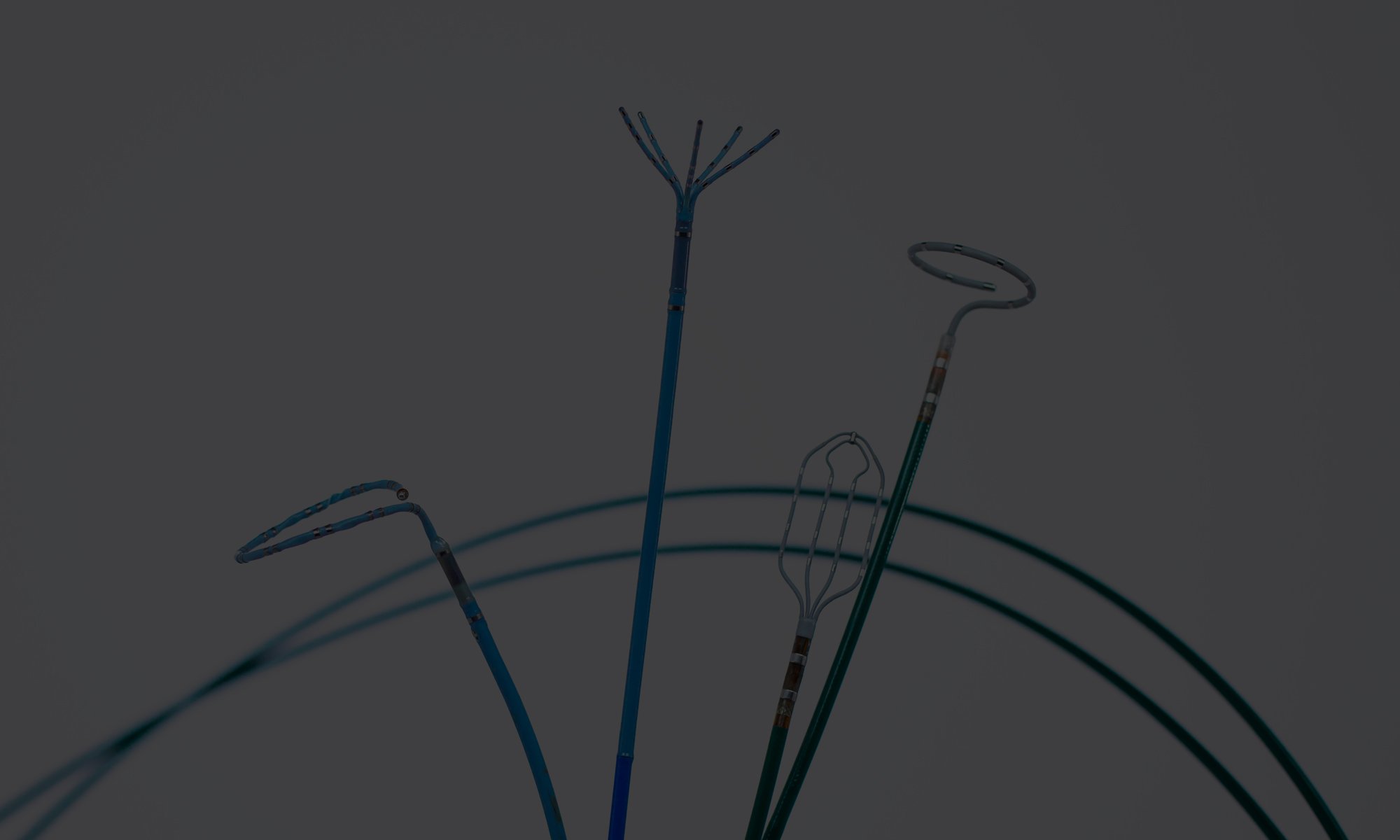
Last year, surgery centers saw CMS add 11 new procedures to the list of ASC payable procedures. This expansion included many orthopedic procedures that had traditionally been performed in the hospital setting. In addition to the 11 new procedures, CMS issued the ASC Payment system proposed rule which included a timeline for the elimination of inpatient-only procedures by 2023. This aggressive push by CMS looked to move a significant number of cardiac, spine and urology procedures into the Ambulatory Surgery Center setting in 2022. When the CMS issued the list of new procedures under the 2022 Outpatient Prospective Payment ruling, many of those proposed changes and several already approved procedures had been moved back to the inpatient only list. Only two cardiac procedures made the list of outpatient procedures: Diagnostic heart caths and simple stenting procedures. The reversal by CMS was based on feedback from physicians and professional organization that cited concerns about patient safety and appropriateness. In the cardiac space, these clinical concerns are a) perceived concerns about the unknowns in a procedure; b) the potential escalation of simple diagnostic procedures to complex interventions; and c) reimbursement margins that are already small in the inpatient setting (Condon, 2021).
Only two cardiac procedures made the list of outpatient procedures: Diagnostic heart caths and simple stenting procedures.
Many of the cardiac procedures that were removed from the list have a high degree of variability. This means that every case is different, and it becomes difficult to predict which cases should be moved into the ambulatory setting. While the ambulatory setting has been successful at reducing costs in many cases, this also comes with reduced access to support services: Ancillary services are not available onsite at these facilities. The facilities lack the ability to perform lab work, imaging, or ultrasound services. Instead, they are focused and specialized with only the equipment necessary to perform the surgeries. This specialization is what has allowed the surgery centers to remain effective at reducing costs, but it also limits the ability to pull in additional resources when needed. Many cardiac patients have multiple disease states and significant co-morbidities. This makes it challenging when trying to select patients for the ambulatory setting and is concerning for cardiologists who currently are doing all procedures regardless of patient selection in one location that offers all the necessary ancillary services.
Ambulatory surgery centers have seen success performing routine procedures, meaning surgeries or procedures that have very little variance is the perfect target. The costs are relatively understood and fixed before the procedure starts, and there is little or no technical variance during the procedure. Percutaneous procedures that have traditionally been done in the cath lab do not fall into this category. They tend to start with a diagnostic portion that determines if something needs to be stented or repaired, and it is difficult to predict prior to the start of the procedure which patients will need simple procedures, and which will need complex ones. This variability and expectation that a certain percentage of cases will become more complex than anticipated creates challenges when looking to transition cardiac procedures into the ambulatory setting. In addition, concerns about what happens when a simple procedure becomes complex, complications that occur in cardiac procedures can quickly become life threatening needing emergent surgical intervention. This seems difficult enough when the operating room is down the hall from the cardiac cath lab, having the patient miles way from the closest acute care hospital makes this even less appealing to proceduralists.
The third consideration when moving some procedures into the ambulatory setting is profitability. Since Ambulatory surgery centers receive lower reimbursement than hospitals for identical procedures, profit margins are important. Cardiac procedures in the hospital setting generate good revenue for the organization when you look at all the procedures together. Heart caths, ablations, device implants and structural heart cases combine to generate massive revenue for hospitals. But when you start to peel of the procedures that are likely to be performed in the ambulatory setting the margins quickly diminish. For instance, in the ASC, CMS pays on average $1,702 for a diagnostic angiogram/heart cath, but a hospital gets paid $3,198. With such a discrepancy in reimbursement these procedures no longer remain profitable for the Surgery Centers (Ambulatory Surgery Center Association, 2021) – while hospitals lose the procedures they needed for their profitability.
Since Ambulatory surgery centers receive lower reimbursement than hospitals for identical procedures, profit margins are important.
There is no doubt that the cost of cardiac procedures needs to come down. There is also little doubt that more predictable, less risky procedures should be performed outside the hospital – to reduce the overall cost of care. However, a simple ASC model for this has proved problematic, and as illustrated, CMS has been all over the place in terms of creating a reasonable incentive for this transition. We need to take a closer look at the full range of cardiac procedures, and then look at how an ASC model can be modified to reflect the realities of cardiac treatments. The current model is not going to work in the long run.
References
Ambulatory Surgery Center Association. (2021). 2022 final medicare payment rule released; minor improvements but still disappointing. Retrieved from https://www.ascassociation.org/asca/aboutus/latestnews/newsarchive/newsarchive2021/november2021/202111medicare2022finalpaymentrule
Condon, A. (2021). CMS finalizes 2022 rules with 255 procedures removed from ASC-payable list. Beckers ASC Review, Retrieved from CMS finalizes 2022 rules with 255 procedures removed from ASC-payable list