Fixing the Disruption
Reprocessing and supply chain resilience
Supply chain resilience used to be the concern of supply chain leaders and operators. Today, it is something that everybody is talking about. The pandemic (and other events, such as the strained US-China relationship) helped us realize the critical importance of supply chains - and its impact on everything and everybody, from the availability of sanitary wipes to the provision of healthcare services, helped democratize the discussion. We all understand that when healthcare workers don’t have masks, they can’t keep you safe; and when hospitals can’t buy critical devices, they can’t perform surgeries. The vulnerability of the healthcare supply chain has become an area of particular interest. This is because of two things: 1) overwhelmingly, the healthcare supply chain has not been designed to be resilient, it has been designed to be efficient - and the cost of this lean approach became brutally clear during the pandemic; and 2) while a non-resilient supply chain in (for example) the car industry is impractical and financially problematic, a non-resilient supply chain in healthcare can postpone procedures, change outcomes, or even cost lives.
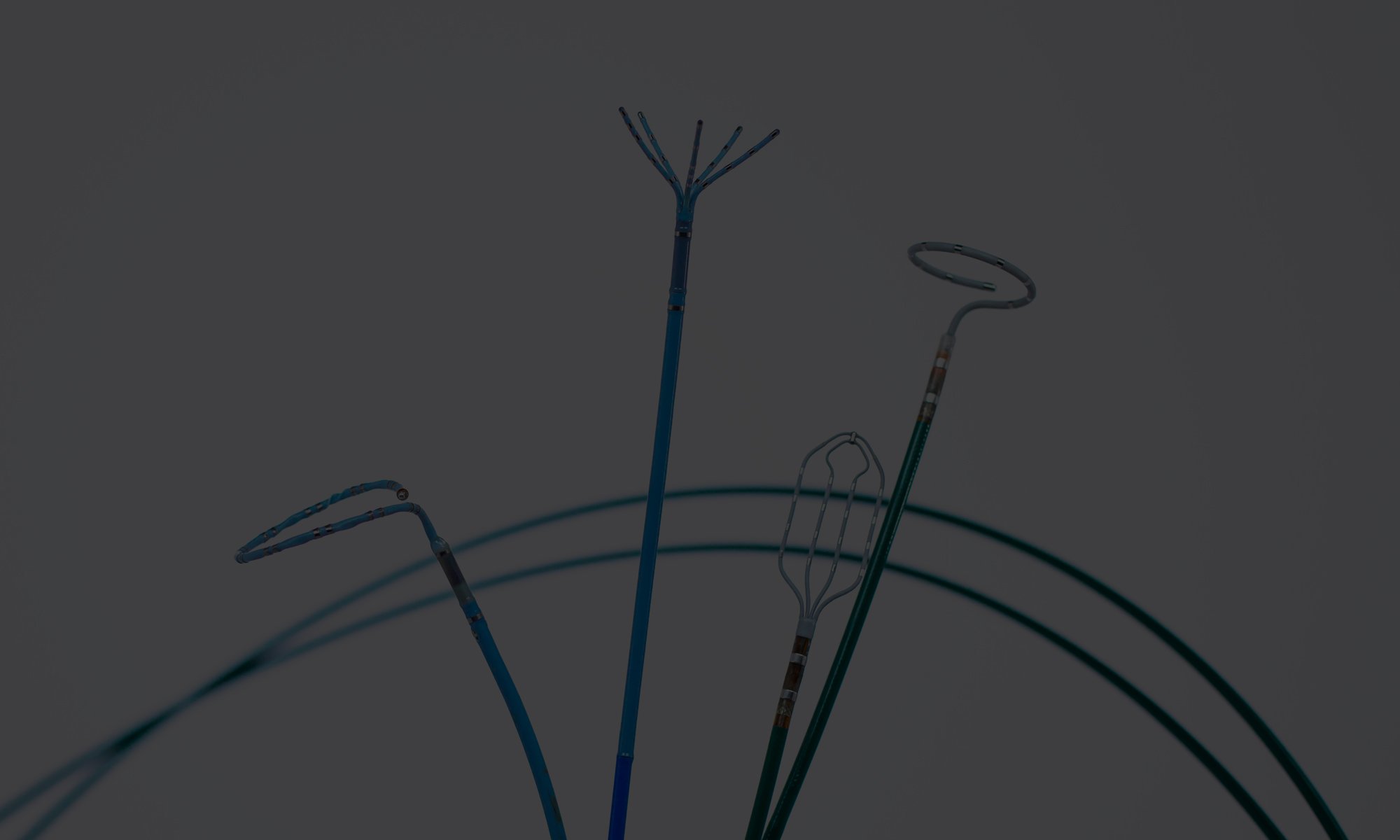
During the pandemic, all eyes were on masks, gloves, etc. – focus was on caring for critically ill COVID 19 patients. Many procedure areas were on hold or had slowed down. Today’s supply chain resilience discussion is about something else: It is about instruments and devices needed for standard procedures in areas such as cardiology, orthopedics, etc. There is a chip shortage, certain materials to produce the devices are unavailable, etc. – and as a result, providers (hospitals) are struggling to make procedures available to patients. For example, in an Atrial Fibrillation procedure, one of the most common and fastest growing cardiology procedures, catheters and other devices used to diagnose and treat Atrial Fibrillation are inserted through introducer sheaths. These sheaths, while relatively simple in their design, are needed to perform the procedure. One of the largest US providers of introducer sheaths has recently placed the device on backorder due to component/material shortages – hospitals simply cannot buy them. When hospitals cannot buy a device critical to a procedure, they can either a) ask the doctor to use a different device that he/she may be less familiar with; or b) not perform the procedure.
One of the largest US providers of introducer sheaths has recently placed the device on backorder due to component/material shortages...
While switching to a different device that does the same thing sounds obvious, it is not so in healthcare, certainly not in cardiology. Cardiologists (Electrophysiologists) have typically been trained on a certain mapping system, and their device preferences are dictated by the reliance on one mapping system. This is what they are used to, these are the devices they have used hundreds of times. Switching to another introducer sheath, mapping catheter or even diagnostic catheter is not like switching from Pepsi to Coca Cola. All brands of electrophysiology devices are different from one another, and making the switch may result in an impact on procedure time or outcome. It certainly results in physician dissatisfaction.
However, in cardiology as well as in certain other procedural areas, there actually is a third option: c) use a reprocessed sheath (or other devices), avoiding procedure postponement without changing the device used. In addition, procedure costs are reduced by 100s of dollars. This is why reprocessing and other healthcare re-use models need to be considered key healthcare resilience strategies – they bridge the gap between clinical preference and device availability – they enable providers to move ahead with procedures, even if the original manufacturer has placed the device on backorder. Today, we experience hospitals placing orders for reprocessed introducer sheaths, even if the physicians have in the past felt a bit uncomfortable about using them. As a result, procedures are moving forward, doctors are happy, and patients get the appropriate care.
...procedures are moving forward, doctors are happy, and patients get the appropriate care.
In general, making the healthcare supply chain more resilient requires new, radically different – and sometimes uncomfortable - supply chain practices:
- Multi-sourcing – electrophysiology labs often work with only on major supplier of systems and devices. This is driven by physician preference as well as short term supply cost considerations. However, as discussed in this University of Central Lancashire article, “[t]he implementation of lean initiatives and single-sourcing policies, for example, may help to cut costs and improve coordination, but they may also leave a supply chain with no spare capacity to cater for contingencies and therefore susceptible to disruption” – labs with more than one supplier (mapping system) have a more resilient supply chain (and more bargaining power).
- Re-use – re-use models are not popular in healthcare, because they are intuitively associated with higher patient risk. However, single-use device reprocessing is a re-use model that is FDA regulated and has a 25-year safety record in the US – using reprocessed devices do not increase risk of patient harm. Re-use (circular) models enhance resilience because device raw material is derived from the user, not from an external, often distant, source. In this case, a reprocessor can supply the lab with introducer sheaths that are FDA cleared, thereby immediately fixing the supply disruption without challenging physician preference or sacrificing safety.
- Transparency – increased healthcare supply chain resilience also involves more data sharing, more transparency, so that the different channel partners can understand, anticipate and prepare for shortages or disruptions. This point was made in a recent AHA Transformation Talk: “There will be a greater need for bidirectional transparency and greater sharing of utilization data among health care providers, manufacturers and distributors.” Hospitals that share their utilization data with the reprocessor (and others) are capable of reducing risk in the supply chain.
- Pre-planning – Just-In-Time (JIT) ordering has become the standard in many hospital operations. This allows the hospital to save space and improve cashflows. However, similar to single-source supplier relations, JIT ordering comes with inherent challenges to the solidity of the supply chain: Disruptions have immediate impact – there is no buffer. Creating a buffer in terms of storing supplies may not be a long-term solution to disruptions, but it sure helps in the short run.
After the pandemic, hospital leaders have started focusing more on supply chain resilience. The Healthcare Industry Resilience Collaborative was formed, and providers are increasingly asking suppliers to demonstrate supply chain resilience. However, providers (hospitals) must look at their own practices, as well, and dramatically alter the way devices are purchased and used.