Does Better Medical Technology Mean Better Patient Care?
At first glance, you look at the technology itself, and it truly is impressive how manufacturers in the space come up with new methodologies, functionalities and designs every year. But it’s not just about the technology itself. It’s also about how the new technology impacts our ability to care for every patient who needs it. The patient on the table, the patient who isn’t a patient yet, and the patient that never made it to the table because providers couldn’t afford it. The use of expensive technology doesn’t just impact the patient on the table.
The use of expensive technology doesn’t just impact the patient on the table.
The doctor’s decision-making impacts the ability of the healthcare system in general to care for all patients and it impacts the environment. In addition to a focus on the individual patient, the physician must balance the individual patient needs with the needs of the entire population in a way that ensures financial and environmental resources are not inadvertently depleted. In both cases, we only have a limited amount.
Here are a few concepts that can help us understand this balancing act:
Functionality and efficacy:
New technology is typically celebrated because it has a functional advantage over older technology. However, better functionality does not always mean better efficacy or safety. The SoundStar 3D diagnostic ultrasound catheter was introduced to healthcare with a significant functional advantage: Older technologies created 2D images, while the SoundStar created 3D images. And the technology was rapidly adopted by doctors. 3D is better than 2D. However, it doesn’t necessarily make patients safer or ensure that more procedures are successful. In fact, doctors at some of the most prestigious institutions in the country are still using 2D. Why? Because they do not need the extra functionality to complete their cases successfully. We forgot to ask if better functionality translated to better outcomes.
...better functionality does not always mean better efficacy or safety.
Bostic Scientific’s Farapulse was launched at the conference this year. Instead of ablating using cryo or heat, it ablates with electric pulses. The ablation catheter is also twice as expensive as older technologies. It DOES something better, there is no doubt, and it is theoretically also safer for the patient. But electrophysiology ablation procedures were never very dangerous for the patient, and we really haven’t seen that Farapulse produces better outcomes. Again, we embraced the new technology because it IS better. Not because it DOES better.
Cost and value:
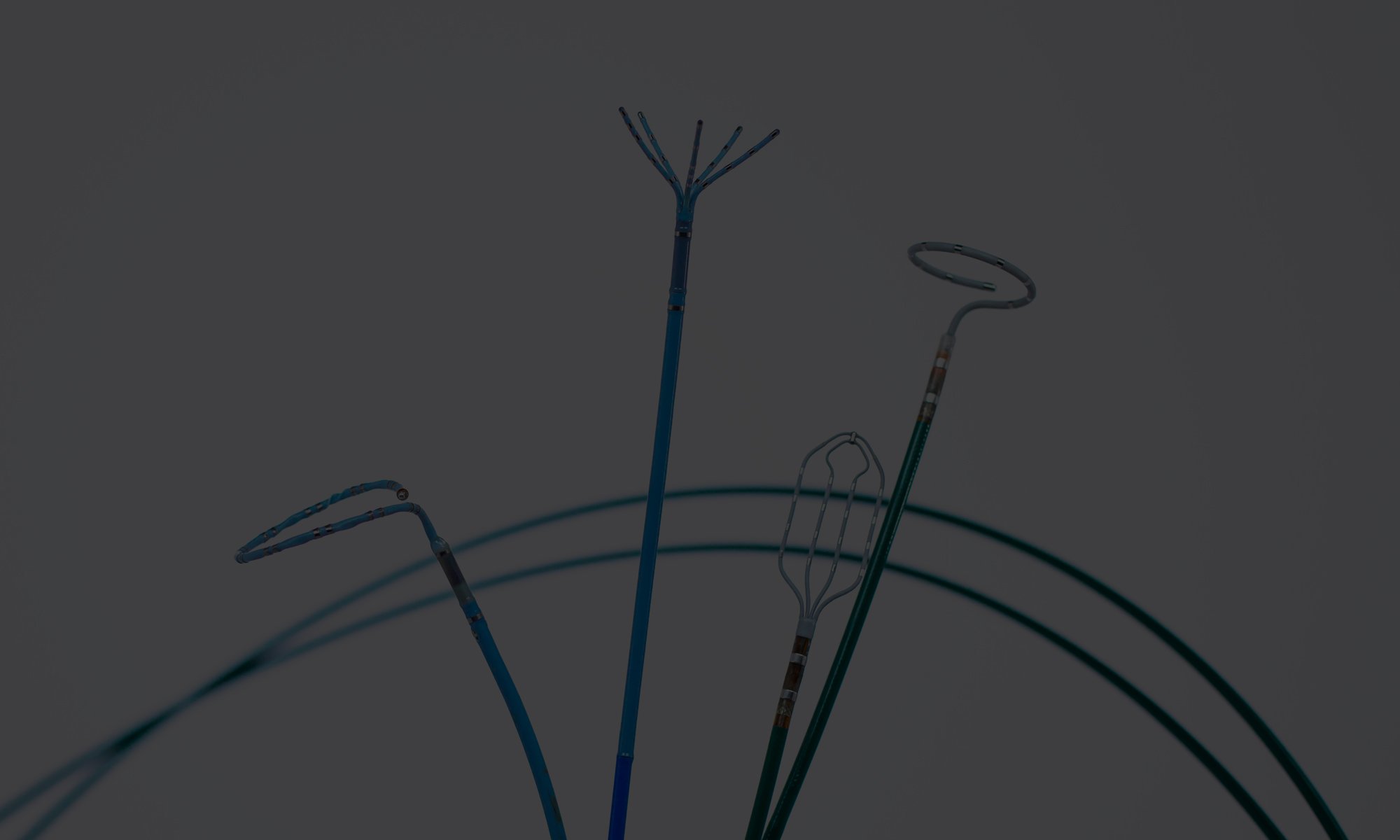
New generations of cardiology devices are always more expensive than the technologies they replace. When the Pentaray mapping catheter was introduced, it was considerably more expensive than the much less advanced catheters it replaced. It’s called the Pentaray because it has five tentacles that aid in the mapping of the heart. It’s been around for a while, and I am sure it is a great catheter – what I don’t know is if the “greatness” justifies the extra costs. A few years ago, the next generation mapping catheter was introduced – the Octaray. Yep, you guessed it. EIGHT tentacles. And much more expensive. Eight is more than five, but does the value of the three extra tentacles justify the extra costs? In South America, they can buy the Octaray. But they don’t. They use pre-Pentaray mapping catheters, because they are less expensive so they can afford to treat more patients…
Utilization and acquisition:
Healthcare is infected with a single-use mentality: If I throw away a device after a single use, there is less risk of cross-contamination. As a result, manufacturers launch more and more devices with single-use labels, in spite of the fact that it goes against everything healthcare is trying to do right now, specifically reducing costs and environmental harm. In cardiology, some single-use devices cost more than $3,000 dollars and the carbon emission footprint of each device can by 2 pounds or more. Buy, use once, then throw away. This is not a balanced practice. The environment suffers, and perfectly good devices are thrown away, forcing the hospital to spend money on another one for the next procedure.
Buy, use once, then throw away. This is not a balanced practice.
Single-use devices can be reprocessed by advanced third-party reprocessors, but, more importantly, they could probably also be designed for safe re-use, reducing environmental harm and hospital costs – possibly improving our overall ability to provide proper patient care.
However, in spite of the obvious logic, manufacturers of cardiology devices are marching in the exact opposite direction. They design obsolescence into devices to avoid them being reprocessed. And more and more cables used in cardiology procedures (yes, cables – cords that don’t touch the patient) are launched as single-use – and they often cost hundreds of dollars, if not more.
In electrophysiology, innovation is king, but it is often incremental, and it almost always lacks rational, comprehensive clinical documentation and relevance for hospitals that try to balance the increasing costs of new technology with increasing demand and reimbursement that just can’t keep pace. It is almost as if the scientists, technologists, and clinicians of the space celebrate innovation for the sake of innovation. The mindset of the electrophysiologist is highly scientific, so it is no wonder technology innovation is a constant focus, but others must temper the pace of innovation with the sobriety of how to address the increasing number of AFib patients with solutions that are both clinically superior and financially and environmentally responsible.
Innovation needs to be balanced with very real concerns about the financial and environmental sustainability of new technology. It is worthwhile asking if the benefits of new technology outweigh the increased financial pressure it will bring to labs and hospitals across the country. Somehow, we need to get to an innovation effectiveness index that can guide the electrophysiologist and help him/her understand the incremental clinical value vs. the incremental cost increases.