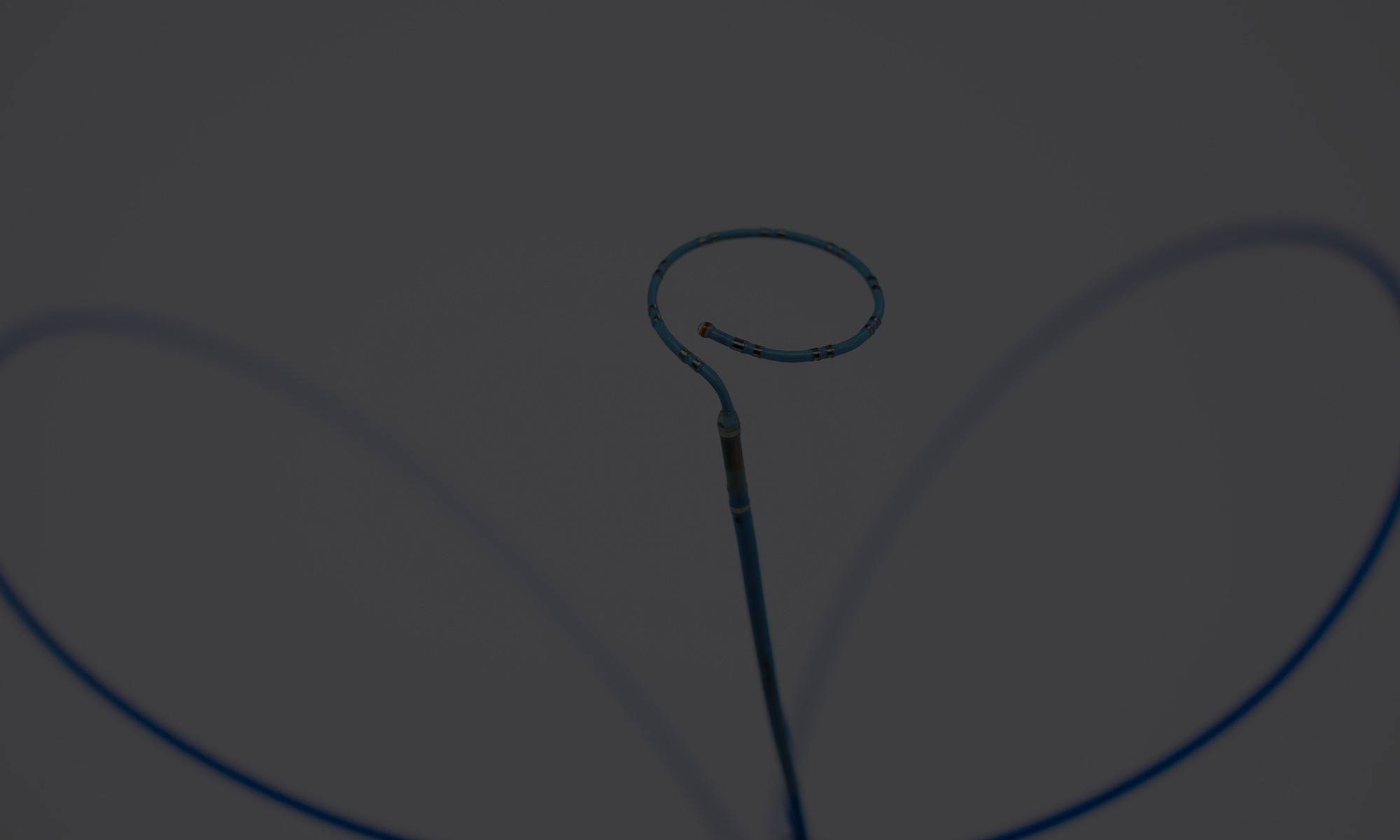
Democratizing Technology in Atrial Fibrillation Ablation
In EP Lab Digests’ September issue, Bradley P. Knight, MD, FACC, FHRS, Editor-in-Chief wrote in the Letter From the Editor, “Any technology or technique that is better, safer, or faster will only be adopted if it is at least cost neutral.” Dr. Knight continues to stress the importance of reprocessing, which plays an important role in reducing per-procedure costs. New electrophysiology technology should always be better and less expensive. We would add another dimension: New technology should always be incrementally more accessible to doctors and technologists. And this is a challenge in electrophysiology.
New technology development in electrophysiology is very rapid: As Atrial Fibrillation and other EP related diagnoses continue to grow in the US population, medical device manufacturers focus more of their investment dollars on this treatment area. This is, of course, because technology can enable us to make a difference in the treatment of these diagnoses – but it is also because this is how manufacturers can maximize their revenue: The shorter the technology life cycle, the more frequent the introduction of new devices. And since new device launches usually are associated with price increases (you can charge more for a better technology), the chase to treat patients better has produced a rapid upward spiral on prices and, therefore, costs to the hospital. This is the cost problem mentioned, and focus should be on making new technologies less expensive, not more expensive. It is already a challenge for many rural hospitals or hospitals with an unfavorable payer mix (more Medicare patients, fewer with private insurance and higher reimbursement for the hospital) to provide electrophysiology services to all the patients that could benefit from them.
...the chase to treat patients better has produced a rapid upward spiral on prices and, therefore, costs to the hospital.
The rapid technology development has other consequences. Electrophysiology (EP) is not exactly a new field, but its adoption has been relatively slow. This means that while some EP doctors are magicians with EP devices and can complete successful cases in a few hours, many other EP doctors do fewer cases, are less used to the procedures, and spend less time with the devices and the technology. The result is great variation in the knowledge of EP technology and ultimately in the proficiency of doctors: It is tough to become an expert on procedures and devices that you only encounter once a week. This, in turn, can mean that procedures take longer, become less financially beneficial to the hospital, and result in a lesser patient outcome. This problem is exacerbated by the rapid technology development: Some clinicians and technologists are simply unable to catch up when a new mapping technology is launched or a new generation ultrasound system is introduced – if the hospital can even afford the new systems/devices.
In other words: There is a trade-off between technology advancement and technology accessibility. When new functionality is added to EP devices, when mapping software becomes more accurate, and when new devices come with more options, technology complexity grows, and successful use of the new technology requires more and more expertise and experience on the part of EP doctors and technologists. Because these new technologies are also more expensive, adoption is slower and many procedures are completed with last-generation technology. In many cases, this is actually ideal, since all the newest functionality isn’t needed in every case, but it does prevent the market from benefiting optimally from new technology.
There is a trade-off between technology advancement and technology accessibility.
Instead of designing technology solutions that benefit the most advanced doctors and labs, medical device manufacturers should focus on technology access. The question should not only be “How do I develop a new technology that can do more?” The question should also be: “How do I design a device that is easy to use for a doctor at a small rural hospital in Montana?” There is a case for technological advancement to slow down to let the market catch up, but technology development doesn’t necessarily have to slow down. Several smaller companies in the EP space have started focusing on the democratization of technology, deliberately looking at user experience, automation and procedural standardization as high priority design goals: The more the technology can do itself, rather than relying on clinical expertise, the more accessible the technology. And the industry’s ability to appropriately meet the increasing demand for Atrial Fibrillation procedures depends on this.