Ablation Procedures in Surgery Centers?
When things go wrong in a procedure, you most certainly want to be in a hospital, simply because the capability of a hospital to address major adverse events in a procedure is immensely higher than the capability of a surgery center to address the same (this is also why most surgery centers are located close to a hospital). However, EP ablation procedures are actually quite safe. Cardiac perforation causing tamponade is the most common adverse event from EP ablation procedures, and while it can be deadly, electrophysiologists can actually usually handle these emergently. Studies show that adverse events in EP ablation procedures is actually far less than in other procedures, such as orthopedics, that has already moved to the surgery center setting.
But, even if the risk is minimal, why take a risk at all? Well, procedures done in the surgery center are much less expensive and are usually associated with high financial award for the electrophysiologist (who is often a co-owner of the surgery center). Interestingly, one of the drivers behind the growth in surgery center ablation is the fact that the Centers for Medicare & Medicaid Services (CMS) has reduced physician reimbursement significantly in recent years.
Surgery centers can do EP ablation procedures much less expensively because they are run more like businesses than hospitals that, as large institutions with high degrees of complexity and administrative burdens, waste a lot of resources. Surgery centers are often run by business executives who know how to create efficiencies while also providing high quality care. I have actually heard several hospital executives admit that they “would like to learn how to do healthcare from the surgery centers”.
I have actually heard several hospital executives admit that they “would like to learn how to do healthcare from the surgery centers”.
Here is what to expect when we, in a matter of months, see substantial growth in the number of EP ablation procedures performed in surgery centers – outside the hospital:
- CMS will not issue reimbursement codes for ALL EP ablation procedures in 2026. Rather, it will likely issue reimbursement codes for ablation procedures that are less complex (less risky). This will correspond with the appetite of the electrophysiologists, who will also not want to do the most complex procedures on day 1 in the surgery center. The elderly AFib patient with lots of co-morbidities will likely still be treated at the hospital. Similarly, many re-do procedures (lots of ablation procedures are not successful on the first attempt) will probably also be done in the hospital. CMS will then gradually add codes as the migration proves to be successful.
- We will see new approaches and methodologies to EP ablation emerge and evolve in the surgery center setting. This is because of the type of procedures initially moved into the surgery center – they are less difficult, likely faster, and require less technology. Add to this that the electrophysiologists are financially incentivized and will approach their methodologies with a different mindset than the hospital reimbursed doctor. This will lead to interesting – and useful - new developments. The best manufacturers of ablation technology are watching some of these doctors carefully to see what will happen when ingenuity meets financial incentives.
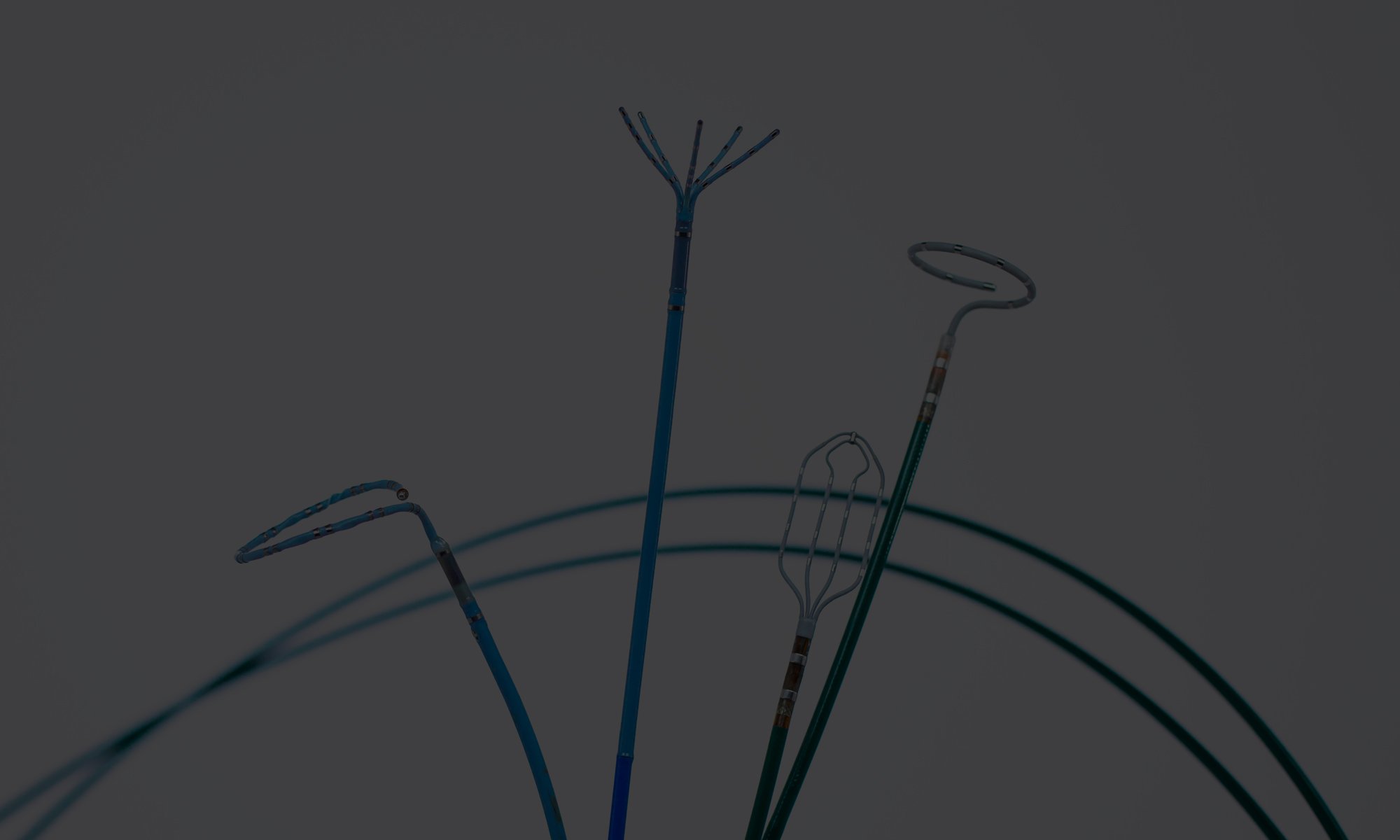
- It follows that we will see new technologies for EP ablation emerge and develop in the surgery center. In fact, some will argue that already the launch of Pulsed Field Ablation (PFA) technology in the EP space pre-empts the migration of EP ablation to the surgery center (and the different mindset and procedure conditions of this setting) with EP ablation technology that allows for faster and safer procedures.
- PFA-based ablation procedures will also allow for procedures that use fewer devices and have reduced complexity, thereby driving down costs. We will see new technologies that make it easier to either switch between brands or completely eliminate the need for devices – in both cases optimizing clinical choice and efficiency. This is an interesting reversal of the situation in the hospital, where procedures are typically overloaded with devices to allow for multiple visual modalities and (arguably) excessive procedure steps. Much of this will be dropped in the surgery center. Mind you, this doesn’t mean you get a “lesser procedure”, it simply means that what was unnecessarily utilized and paid for is no longer included.
- Some of the best electrophysiologists in the country are going to be among the first to start doing procedures in the surgery center. They are the physicians who are skilled enough in their practice to want to do procedures without excessive equipment, who are confident enough in their practice to develop new perspectives and methodologies. These physicians will have a different mindset due to who they are, but also due to WHERE they are. They will be performing simpler procedures in less time, utilizing less devices. They will also be making more money, and their choice of methodology, approach and technology will be impacted by the fact that they have financial interest in the profitability of the surgery center.
- Finally, we will see more device re-use: Single-use device reprocessing is already of key importance to the financial sustainability of hospital-based procedures – in the surgery center, the physician’s legacy preference for a brand-new device will be replaced by the financial appeal of a reprocessed devices that can be acquired at half the price.
The fragmentation of care setting that we experience with the migration of procedures out of the hospital is ultimately a good thing. It makes healthcare less expensive, eliminates inefficiencies and creates the kind of competition hospitals have never really had.