A Biomedical Engineer’s Perspective on Reprocessing Single-Use Devices
As a biomedical engineer coming out of school, my goal was to work for an OEM in the Research & Development (R&D) department creating new products and improvements to existing products. This scenario would allow me the optimal clinical and mechanical balance with a focus on human factors engineering. After reading more about Innovative Health and the reprocessing industry, this OEM-or-bust perspective was challenged. Following the initial interview for an R&D Engineer position, a facility tour was conducted which showcased the different facets of what Innovative Health does as a reprocessor. This also included a brief overview of the extensive and sophisticated processing, testing, and reporting involved in securing a premarket FDA clearance on a reprocessed device. After spending the day at Innovative Health’s manufacturing facility and interacting with the staff, the remnants of any negative perspective or stigma about reprocessing was gone. An OEM was no longer the only option to break into the medical device field as an entry level engineer. Now, the post-graduation job choices included Innovative Health’s R&D department which would allow for more creative freedom, problem solving, and interaction with FDA-facing documentation (this is an engineer’s playground).
After spending the day at Innovative Health’s manufacturing facility and interacting with the staff, the remnants of any negative perspective or stigma about reprocessing was gone.
Now, as an official part of the R&D team at Innovative Health, expectations of what traditional R&D “looks like” have been broken down and enhanced through interactions with the wider team which have brought to light a space where process engineering, reverse engineering, problem solving, project management, FDA documentation, test protocol creation, production processing, and interaction with third parties such as hospital staff and laboratories is all bundled into a single role with extensive cross-departmental communication. While this sounds like a lot on paper (which it is), the multi-functionality of an R&D engineer and application of skills efficiently allows for Innovative Health to advance faster with high-quality product toward 510(k) premarket clearances and successful creation of reprocessing technologies/techniques consistently.
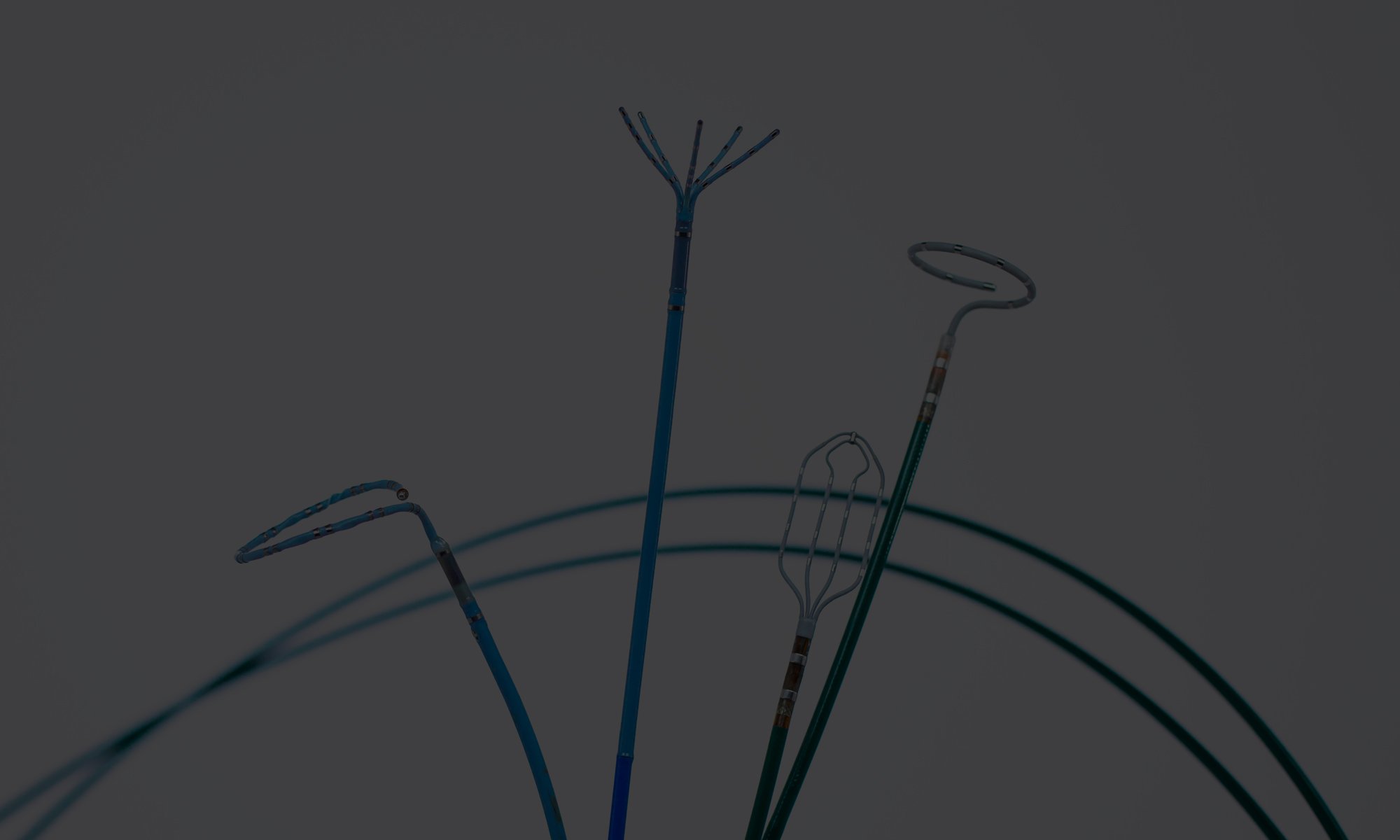
From a non-engineer perspective, hearing “sophisticated processing, testing, and reporting” may not prove the point. To expand on this a little, a device’s journey within R&D follows design control phases of planning, feasibility, qualification, transfer, and post market. The feasibility and qualification phases are where the bulk of the testing and evaluation occurs to validate that the device can be cleaned without compromising product performance or safety. This phase includes, but is not limited to OEM device characterization, risk analysis, test method development, and validation studies to ensure the device is safe to be used in the human body and will function as intended post-reprocessing and sterilization. While this is highly simplified, it is representative of 6-10 months of work per device, not including the additional timeline for the other three phases. Furthermore, due to Innovative Health’s strict quality control and standards, a higher confidence level can be held on device performance. This is because every single device reprocessed by Innovative Health is tested and evaluated individually prior to being shipped for sterilization and inspected again before being shipped to the customer. Compare this with production quality control at large OEMs, who may use acceptable industry standards for batch testing instead. By performing 100% quality control throughout the entire process (collection to finished products), Innovative Health is able keep a record of any given device’s journey through its facilities.
...due to Innovative Health’s strict quality control and standards, a higher confidence level can be held on device performance.
The reprocessing industry is becoming more accepted and celebrated within the medical community, especially now when hospitals are dealing with supply chain constraints due to the global pandemic. Regardless, push-back from physicians and hospitals due to the underlying stigma of reprocessed devices is still expected. This stigma was created during the time when hospitals would re-sterilize single-use devices in their sterile processing department for reuse until they failed, prior to the time when this practice was regulated by FDA. These FDA rules and regulations are there for a reason - to ensure patient safety and efficacy of the device. Through the 510(k) process implemented by FDA, OEMs have to prove the safety and efficacy of new devices through tests and/or data such as performance, biocompatibility, bench testing, sterilization, shelf-life testing, packaging validation, etc. to prove substantial equivalence to a predicate device (a device that is currently used and functions similar to the subject device). After extensive review by FDA, which is expected to be a minimum of 90 days, if all requirements are met to prove safety of the patients and efficacy of the device, a clearance to market and sale of device is issued. With the reprocessing industry being heavily regulated by FDA now, reprocessors are held to the same standards and requirements enforced on the OEMs. With a better understanding of the process, it could be argued that a reprocessor has to meet a higher standard than OEM to prove the safety and efficacy of a device. A reprocessor must prove that a given device can be effectively reprocessed, but also meet all the performance requirements just like an OEM to prove substantial equivalence to the predicate. While those of us who are in the reprocessing industry understand this, an outsider may not, so it does not come as a surprise that there is still resistance to the use of reprocessed devices. However, with continued public education by specialty reprocessors, physician feedback, adoption of advanced (but reprocessed) devices by highly reputed medical systems, independent comparative studies, etc. confidence surrounding usage of reprocessed devices for a positive clinical outcome is only increasing.